Researchers have discovered a distinct microbial signature in the mouths of individuals with obesity, raising the possibility of early detection and preventative strategies. The study, conducted by Aashish Jha at New York University Abu Dhabi, analyzed saliva samples from over 600 Emirati adults, revealing significant differences in the oral microbiome between those with obesity and a healthy weight control group.
The Oral Microbiome and Metabolic Health
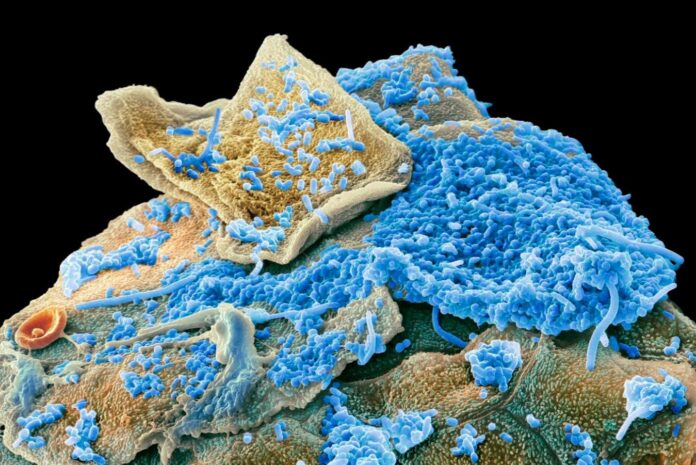
The human mouth harbors over 700 bacterial species, forming the second-largest microbial ecosystem in the body after the gut. While gut microbes are well-known to influence weight gain, the role of the oral microbiome has been less understood. This research suggests that specific bacterial imbalances in the mouth correlate with metabolic dysfunction.
Specifically, obese individuals exhibited higher levels of inflammation-driving bacteria like Streptococcus parasanguinis and Actinomyces oris, as well as Oribacterium sinus, which produces lactate – a compound linked to poor metabolism. The study also found 94 differences in microbial metabolic pathways between the two groups. Obese participants showed boosted carbohydrate metabolism and histidine breakdown, while their ability to produce essential B vitamins and heme (crucial for oxygen transport) was impaired.
Metabolite Patterns and Systemic Effects
The altered microbial activity resulted in elevated levels of metabolites such as lactate, histidine derivatives, choline, uridine, and uracil. These compounds are associated with metabolic disturbances like high triglycerides, liver enzymes, and blood glucose. Researchers described the environment in the mouths of obese individuals as “low-pH, carbohydrate-rich, and inflammatory.”
“This study provides some of the clearest evidence to date that the oral microbiome reflects, and may contribute to, metabolic changes associated with obesity.” – Lindsey Edwards, King’s College London
Causation vs. Correlation
While the findings demonstrate a strong association, establishing whether the oral microbiome causes obesity or is a result of it remains the next step. Jha and his team plan follow-up experiments examining microbe and metabolite transfer between the mouth and gut, hypothesizing that direct bloodstream access via oral blood vessels could rapidly distribute metabolites throughout the body.
It is possible that dietary changes favor certain bacteria, which then produce metabolites influencing cravings and reinforcing obesity-promoting behaviors. For example, uridine is known to increase calorie intake.
Implications for Prevention and Intervention
If a causal link is confirmed, interventions could include oral microbe transplants (via gels), prebiotics, targeted antimicrobials, or pH-modifying rinses. However, even if the oral microbiome is merely a marker of obesity, a simple saliva test could provide early detection, facilitating preventative measures like dietary adjustments.
The study highlights the interconnectedness of microbial ecosystems and systemic health, underscoring the importance of oral hygiene in metabolic well-being. Further research is needed to fully unravel the complex interplay between oral bacteria, metabolites, and obesity development.